Two types of plannings are 1. Capacity planning is the practice of planningdetermining production capacity and workforce needs to make sure your supply chain is equipped to meet demand.
 Process Selection And Capacity Planning
Process Selection And Capacity Planning
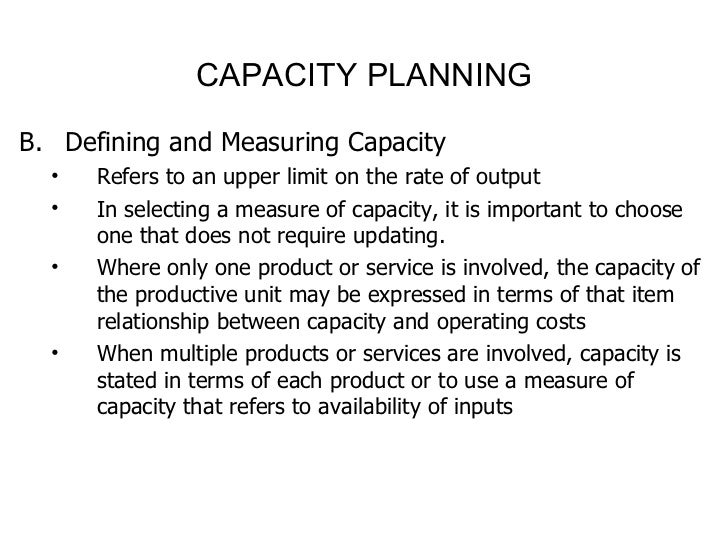
In the context of capacity planning design capacity is the maximum amount of work that an organization is capable of completing in a given period.
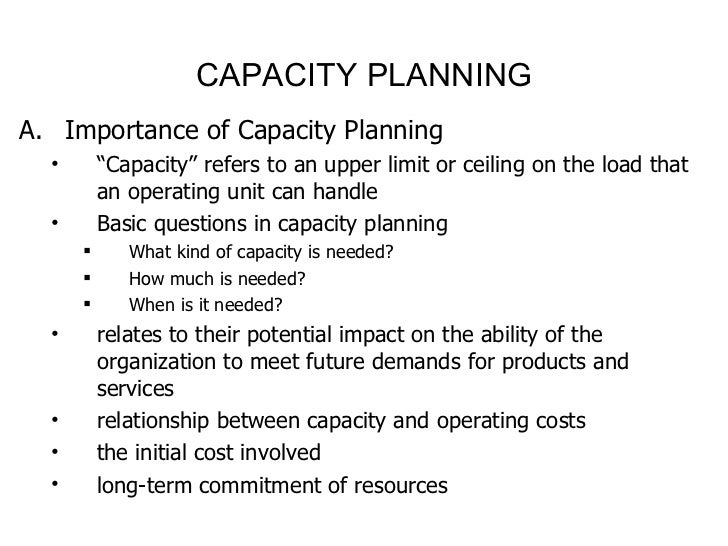
Capacity planning definition. At a project level capacity planning is all about determining whether you have enough resources to complete a given project. Conducting a CRP analysis is a critical management tool. In order to calculate your teams capacity you need to know their availability and their current workload.
Typically capacity planning collects the computing capacity of the current environment and employs statistical and analytical tools to. Check out results for Capacity planning in excel. You just clipped your first slide.
Capacity planning is described as a tool to minimize the discrepancy between the capacity of a business entity and customer demands. Capacity in this case is the most work that can be done over a certain timeframe. In information technology capacity planning is the science and art of estimating the space computer hardware software and connection infrastructure resources that will be needed over some future period of time.
Now customize the name of a clipboard to store your clips. Capacity planning lets businesses know how and when to scale identify bottlenecks create better design capacity and mitigate risk within a planned period of time. Capacity planning is a systematic approach to planning for future IT resources based on current operations demand and growth.
How Does Capacity Planning Help in Sprint Planning. Capacity planning is a process that balances the available hours of teams against what the project needs. Capacity requirements planning CRP is the process of discerning a firms production capacity and whether it can meet its production goals.
Demand for capacity is variable as it is based on changes in production output of an existing product or in the production of a new product. The production system design planning considers input requirements conversion process and output. What is capacity planning.
Rough cut capacity planning is the process of converting the master production schedule into requirements for critical resources. Clipping is a handy way to collect important slides you want to go back to later. Check out results for Capacity planning in excel.
Because capacity decisions often involve substantial financial and other resources it is necessary to plan. Capacity planning is a great way to invest your time because it helps you address possible future issues take advantage of the benefits that come with planning improve team performance and streamline your business tasks for increased efficiency. The word resources may mean people equipment software rooms and so on.
It often includes labor machinery warehouse space suppliers capabilities. Long term capacity planning. Short term capacity planning 2.
Capacity affects the ease of management. Capacity decisions can affect competitiveness. Capacity Planning As I mentioned its used not only in manufacturing its also used as a strategic method.
Capacity Planning is the process of determining the production capacity needed by an organization to meet changing demands for its products Wikipedia in English. Capacity is defined as the ability to achieve store or produce. Capacity planning is the process of determining the production capacity needed by an organization to meet changing demands for its products.
After considering the forecast and long-term planning organization should undertake capacity planning. Globalizationhas increased the importance and the complexity of capacity decisions.